By Claire Bacon, ACN, CNC
Having a healthy liver is vital to counteracting the toxic exposures we get from daily life and our modern diet. A healthy liver plays a huge part in keeping your immune system well, producing normal amounts of hormones and cholesterol, and creating energy. Unfortunately, 90 million Americans have a progressive condition brewing called fatty liver disease. Most people don’t even know it.
Liver disease doesn’t receive much publicity when compared to cancer or heart disease. But guess what? Fatty liver is the #1 liver disorder in the world. And unfortunately, it has been increasing massively over the last two years. What’s notable is that for the 94% of Covid-related deaths who had on average 4 comorbidities, fatty liver disease was most prevalent. In short, people with the worst outcomes had the unhealthiest livers. The various forms of hepatitis, as well as excessive drinking, and excess sugar/carb consumption are common causes of liver problems.
Although the scientific studies are not in full agreement, it appears that men are more likely to suffer from fatty liver disease. And the longer the inflammation goes on, cirrhosis can develop. Cirrhosis is a type of serious liver deterioration that results from a long-standing disease or injury. People with liver cirrhosis are at significant risk for liver cancer and may eventually require a transplant.
Fatty liver and further complications like cirrhosis are largely preventable and reversable. Luckily, through your diet and lifestyle, you can reduce the toxic burdens at play. But you must first have the right information to get you motivated to take charge of your liver health.
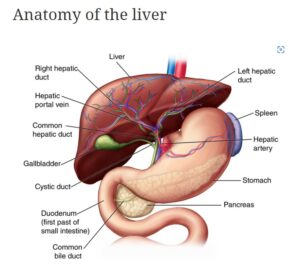
Functions of the Liver
Your liver is your body’s biggest internal organ. It regulates most chemical and hormone levels in the blood. It excretes bile, which carries away waste products through the body. All blood leaving the stomach and intestines passes through the liver. The liver processes this blood and breaks down the nutrients for absorption. It also metabolizes drugs so the body can use them.
In addition, the liver aids digestion, stores energy, and makes blood clotting components. More than 500 functions have been identified with the liver. Amazingly, the liver is able to regenerate or regrow itself to repair damage.
Understanding the Disease State
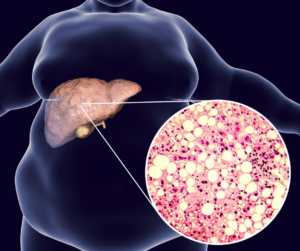
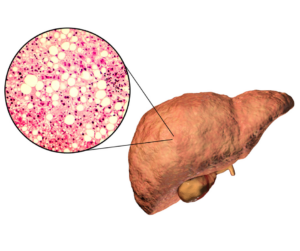
Non-alcoholic or metabolic-associated fatty liver disease (NAFLD or MAFLD) affects approximately 30% of the worldwide population. It is the first step in developing chronic liver disease and cirrhosis. Many other diseases can form, too. NAFLD/MAFLD is the natural result of common, untreated conditions like obesity, dyslipidemia, and Type 2 diabetes.
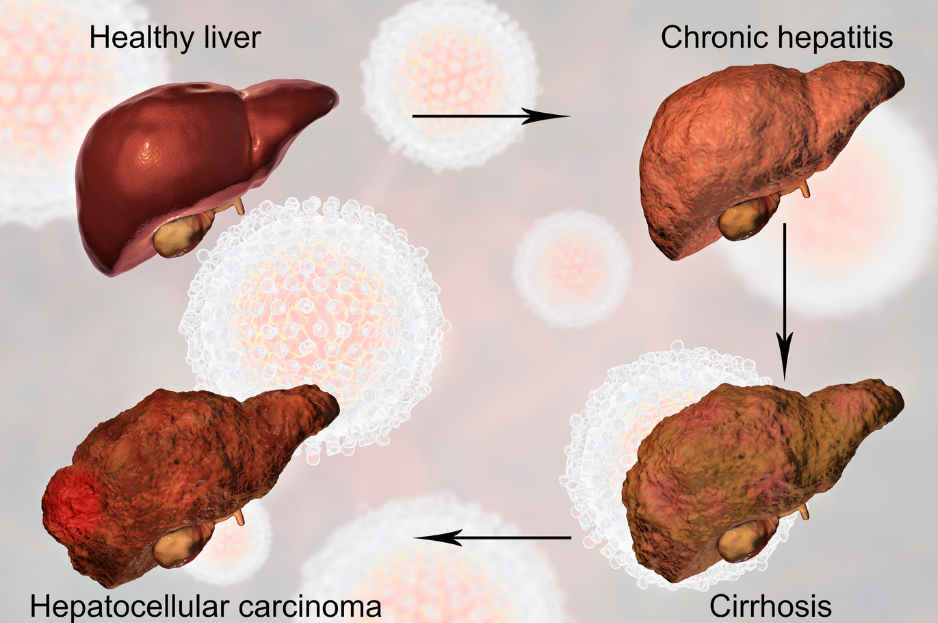
Typically, liver disease progresses through four stages:
- Fatty liver/Non-Alcoholic Fatty Liver Disease: A buildup of extra fat within the liver caused by overeating carbs, too much alcohol, and insulin resistance.
- Steatohepatitis: Increasingly chronic inflammation and cellular ballooning occurs with accumulating fat storage. Usually caused by excess alcohol or certain medications.
- Fibrosis: Chronic inflammation impacts the cellular turnover process, whereby fibrous tissue is put down, rather than healthy new cells.
- Cirrhosis: Extensive fibrosis may turn into permanent scarring and lead to more serious and pathological changes.
Surprisingly, you may not feel any symptoms leading up to the point of fibrosis, except for weight gain. Men will notice an enlarged and hard “beer” belly. Whereas, women may notice fat accumulation on the buttocks. Eventually, as the condition progresses to cirrhosis, you may notice:
- Easy bruising and bleeding
- Unusual fatigue, confusion, and weakness
- Itching skin
- Poor appetite, nausea, and weight loss
- Swelling of the abdomen (ascites) and legs (edema)
- Dark urine color
- Pale stool color (light tan or gray)
- Vomiting
- Yellowing of the skin and eyes (jaundice).

Men are notorious for saying “whatever it is, it will pass” and avoiding going to the doctor. But if you have noticed any of these signs, please – get checked!
Causes of Fatty Liver Disease
A wide variety of triggers can lead to fatty liver disease. These ongoing factors can worsen a fatty liver into cirrhosis. The most common factors are:
- toxic excesses (alcohol, high-fructose corn syrup, or white flour)
- advanced hemochromatosis (high iron storage)
- Infections (hepatitis B and C), and
- autoimmune conditions (autoimmune hepatitis, PBC).
Less common causes include:
- biliary dysfunctions (atresia, stone, tumor),
- vascular conditions (Budd-Chiari, cardiac issues),
- genetic predispositions (cystic fibrosis, lysosomal acid lipase deficiency),
- metabolic conditions (alpha-1-antitrypsin deficiency, galactosemia, Wilson’s disease), and
- iatrogenic disease from another treatment (drugs and medications).
How to Check Your Liver Health?
Unfortunately, liver enzyme blood tests like AST and ALT often don’t elevate in early stages of the disease. As a result, it’s hard to recognize the early warning signs in the blood. In our opinion, the best analysis is to do is an MRI to evaluate the size and fat content of the liver. Typically, the ideal goal for fat content is 2 percent.
Cirrhosis is classified as compensated or decompensated (advanced). Oftentimes, patients with the compensated type may have no symptoms and no abnormalities in lab tests or imaging. Basically, you still feel perfectly healthy.
Decompensated cirrhosis, on the other hand, can occur with symptoms of:
- hepatic encephalopathy,
- variceal bleeding,
- ascites (fluid in the abdomen), or
- jaundice.
Patients with decompensated disease may develop complications involving other organ systems. These may involve: renal failure, hypoxia, pulmonary hypertension, or heart failure.
Treatment of the underlying causes can sometimes revert decompensated cirrhosis back to a compensated (symptom-free) state. If someone does not improve with treatment, they may need to consider a liver transplant.
Malnutrition with Cirrhosis
Oftentimes, patients with a cirrhosis diagnosis may become malnourished. This can happen for a variety of reasons. For instance, he may have a poor appetite and not be eating enough. Or, he may not be fully breaking down his fats. Other reasons for malnutrition could be:
- Discomfort with eating from nausea or ascites (fluid buildup),
- Changes in taste or smell,
- Side effects of medications,
- Ongoing alcohol use,
- Lack of bile acid,
- Effects of portal hypertension,
- Presence of pathogens (bacteria, yeast, or parasites)
- Inflammation from insulin resistance,
- Abnormal amino acid metabolism, and/or
- Increased protein catabolism.
Nutritional Deficiencies with Cirrhosis
In addition to overall malnutrition, patients with cirrhosis often have specific nutrient deficiencies. The most common deficiencies are:
- Fat-soluble vitamin deficiencies (vitamins A, D, E and K) due to impaired bile production
- Vitamin D (as a result of impaired fat breakdown)
- Water-soluble B vitamins, including B1, B6, B9, and B12 due to reduced hepatic storage.
- Zinc – due to ammonia levels being chronically high
- Magnesium
- Branched-chain amino acids
- Iron, often due to lack of hydrochloric acid production and impaired protein digestion.
Anemia is extremely common with cirrhosis, but may be caused by different reasons:
- Chronic inflammation. Liver disease is associated with chronic inflammation, which can cause “normocytic normochromic” anemia.
- Lower erythropoietin levels. The kidneys and liver together produce a hormone called erythropoietin (EPO), which stimulates the bone marrow to produce red blood cells. When the liver is damaged, it may produce less erythropoietin, leading to a decrease in red blood cell production.
- Blood loss. People with liver cirrhosis are more likely to develop enlarged veins in the esophagus and stomach. If the varices rupture, it can lead to severe blood loss, thus causing anemia.
- Hypersplenism. The spleen breaks down red blood cells. People with liver disease may develop hypersplenism (overactive spleen), where the spleen breaks down red blood cells far more quickly than they’re produced.
- Medications. Interferon and ribavirin are often used to treat hepatitis, but can lead to anemia.
Therapeutic Nutrition
Did you know, vegetable protein may be a better choice than animal protein when there is already liver disease. Plant protein has fewer sulfur-containing amino acids and more Arginine and Ornithine than animal-based proteins. To be specific, sulfur-containing amino acids are not tolerable in some advanced forms of disease. For example, Arginine and Ornithine facilitate ammonia disposal through the urea cycle. As an added benefit, the high fiber content of a plant-based diet can help clear nitrogen waste products from the GI tract.

| What to Eat? Foods that promote liver function | What to Avoid? Foods that add burden to the liver |
| Fresh red beets and beet greens | Excess sodium from processed foods |
| Dandelion and other bitter greens | Rancid, low quality fats and fried foods |
| Artichoke | Any form of sugar, soda, or high-glycemic carbs |
| Cruciferous Vegetables (not with encephalopathy) | Nightly alcohol |
| Spices: Turmeric, Ginger, Cinnamon, and Garlic | Eating late night meals |
Helpful Supplements

The main goals of supplementation are to protect liver cells and reduce oxidative stress. In addition, we also want to increase fat burning in the liver. Helpful supplements include N-Acetyl Cysteine, Burdock, and Berberine. Other great herbs include Globe Artichoke and Fringe Tree. In addition, high-dose Omega 3 fatty acids help counteract all kinds of inflammation.
In our office, some of our favorite support products for liver health are:
- Milk Thistle Forte – a concentrated herbal product that supports normal functioning of the liver and protects liver cells from damage.
- Hepatrophin PMG – a specialized extract that provides the cellular blueprints of healthy liver cells. Promotes normal cellular growth and repair.
- Livaplex – is a whole-food multivitamin for the liver, supplying Vitamin A, iron, and zinc to fuel the liver’s normal functions.
- A-F Betafood – a blend of beets mixed with vitamin A and essential fatty acids. It’s the perfect food to keep your liver and gallbladder running well. It’s great to have on hand if you tend to feel sluggish after greasy foods. And excellent to prevent constipation!
- Choline – we refer to this as a “liver detergent”. It helps to stir up toxins and excess glycogen to release them from the liver. Also great for brain function!
Final Thoughts
Have you noticed? We are always talking about liver health! In our practice, we discuss diet, digestion, and elimination constantly. As you know, so many functions within the body can be affected by liver function. Our main goal for you is to always be working on detoxification. We have several ways to accomplish this:
- through our 10-Day or 21-Day Cleanses, watching our diet, and other modes of detoxification like dry brushing, exercising, and sweating.
As we know, liver cells can regenerate. This fact should give everyone encouragement to take action. First step: If you eliminate soda and alcohol from your diet, you’ll be well on your way to better liver health. There’s no better day to start than today!



