By Claire Bacon, ACN, CNC
How do you feel about the word “autoimmune?” Confused? Scared? Discouraged? While you’re looking for answers to your symptoms, daily life can be full of questions. And sometimes it’s hard to get clarity from your doctor. Unfortunately, with long-term symptoms this can lead to chronic dysregulation of the immune system – otherwise known as autoimmunity. Autoimmunity and lupus are not easily identifiable. Flareups can occur in different ways and can elude a diagnosis for years. But when you have an eye out for the patterns affecting the whole body, you can find the relief you need more quickly.
The main function of the immune system is to defend from invading microorganisms, by producing antibodies. These are sensitized types of white blood cells, called lymphocytes. Ordinarily these lymphocytes are prevented from identifying the cells of one’s own body as invaders. With the right conditions, however, immune cells mistakenly attack the very cells they are meant to protect. An interruption of the normal control process can be triggered by bacteria, viruses, toxins, pregnancy and even some drugs and medical interventions. In other words, it appears the inflammation initiated by these agents, whether toxic or infectious, can provoke a “sensitization” (autoimmune reaction) in the involved tissues.
There are over 100 unique autoimmune conditions, and the signs and symptoms are not always clear cut. For example, some autoimmune conditions are organ-specific, as in Hashimoto’s Thyroiditis (thyroid), Psoriasis (skin), or Addison’s disease (adrenals). In non-organ-specific disorders, autoimmune activity is widely spread throughout the body. Examples include Rheumatoid Arthritis (RA), Systemic Lupus Erythematosus (SLE), and Multiple Sclerosis (MS). Here, we’ll explore the potential symptoms and our nutritional strategy for supporting someone with Autoimmunity and Lupus…
Understanding Autoimmunity and Lupus
There are different types of lupus, each of which cause different symptoms. Systemic lupus erythematosus (SLE) is the most common type. It can affect many different organs of the body, including the kidneys, lungs, brain, and blood vessels. Cutaneous lupus erythematosus (CLE) affects the skin. Neonatal lupus is a rare condition in pregnant women that causes the baby to be born with a rash, liver problems, and sometimes a heart defect.
People who have lupus often develop symptoms similar to that of the flu – feeling very tired, sometimes with headaches and a fever, and joints can become swollen or painful. Because similar symptoms can occur with other diseases, such as arthritis, fibromyalgia, and thyroid problems, lupus can be very difficult to diagnose. Its vague symptoms are also why lupus is sometimes called “the great imitator.” It can be a “catch-all” when symptoms and testing are confusing. It’s frustrating but understandable that a proper diagnosis can sometimes take years to figure out.
Lupus Diagnosis
Doctors diagnose lupus based on criteria that include joint pain, rashes, mouth sores, sun-sensitive skin eruptions or worsening symptoms, and a positive antinuclear antibodies (ANA) test. This test identifies a variety of antibodies that can attack healthy cells in your body.
The many different ways lupus can manifest can lead to slower diagnoses. For instance, people may have “incomplete lupus” where they meet some but not all criteria. Similarly, mild symptoms might come and go. Others might have a slow progression, with one symptom initially and others develop over time. Presenting with a rash and joint pain is somewhat standard, although no two cases are ever alike.

Types of Rashes
Lupus that affects the skin (CLE) comes in different forms, and causes different types of rashes. Discoid lupus occurs in people with chronic cutaneous lupus. It produces a coin-shaped red, scaly rash on the cheeks, nose, and ears. Fortunately, the rash generally doesn’t itch or hurt, but can sometimes leave discoloration. If the rash is on the scalp, hair loss may occur.
When systemic lupus flares up, it may produce a sunburn-like rash on the face. The rash is distinctive for its butterfly-like appearance. It spreads across the nose and fans out on both cheeks. Interestingly, this rash can also emerge on parts of the body often exposed to the sun, such as the arms, legs, and trunk. Having a flareup like this can increase photosensitivity, so take care when in the sun.
Cardiovascular Complications
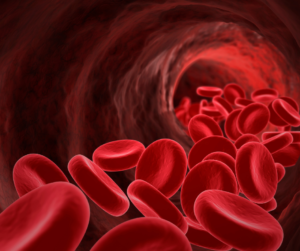
In autoimmunity and lupus, sometimes the attack can damage healthy red blood cells, causing hemolytic anemia. In other words, having too few red blood cells can lead to fatigue, shortness of breath, and/or dizziness. It can even cause a yellowish color to the skin and eyes (jaundice).
Some people with lupus have another problem with their blood. In lupus, thrombosis is more likely, increasing chances of clots to form. This can be very dangerous, and requires immediate medical attention.
Attack on the Nerves, Lungs and/or Kidneys
Lupus can attack the nerves, which carry messages from the brain to the rest of the body. Symptoms vary widely, with headaches, confusion, vision problems, mood swings, dizziness, and/or numbness.
When lupus attacks nerves to the hands and feet, it can cause Raynaud’s phenomenon, which causes the fingers and toes to turn red, white, or blue, and feel numb or painful. Typically, this usually happens in response to cold or stress.
Sometimes lupus can inflame the membrane around the lungs (pleurisy). As a result, this can make breathing painful. In addition, lupus can lead to pulmonary hypertension, where the blood vessel connecting the heart to the lungs thickens. Because blood flow is reduced, the heart has to work much harder to keep up.
Unfortunately, as many as 40 percent of all people with lupus may develop kidney-related complications. Because of the reduction in function, fluid can build up in the legs, ankles, and feet.
Appropriate Diet for Autoimmunity and Lupus

As we have discussed previously, the Autoimmune Protocol (AIP) Diet is most appropriate for any autoimmunity and lupus. This diet is very restrictive, but achieves the goal of being incredibly hypoallergenic. The list of foods to eliminate is pretty long:
- Top food allergens: wheat, dairy, corn, and soy
- Nuts and seeds
- Legumes: peas, peanuts, and chickpeas
- Chocolate and carob
- Nightshades: tomatoes, eggplant, white potatoes and bell peppers.
- Certain herbs and spices, like cayenne, chili pepper, curry, fennel, fenugreek and mustard seed.
That may seem like a lot! But, there are still many hypoallergenic choices you can have. For example, the main items in your diet should include:
- Slow-cooked meat, because it is easier to digest. Also fish and shellfish.
- Most vegetables like broccoli, cauliflower, Brussels sprouts, turnips, beets, and zucchini
- Dark leafy greens like Swiss chard, kale, turnip greens, collard greens, and other dark lettuces.
- Fruit (always organic)
- Homemade bone broth
The goal is to follow a hypoallergenic diet a long enough period of time to bring down inflammation. However, this time period may vary between people. In the meantime, consuming healing nutrients should help reestablish a healthy mucosal layer. This helps maintain a living microbiome that can maintain gut integrity. At some point, reintroduction of foods should be possible without causing flareups soon after. Above all, healing is key!
Th1/Th2 Balance
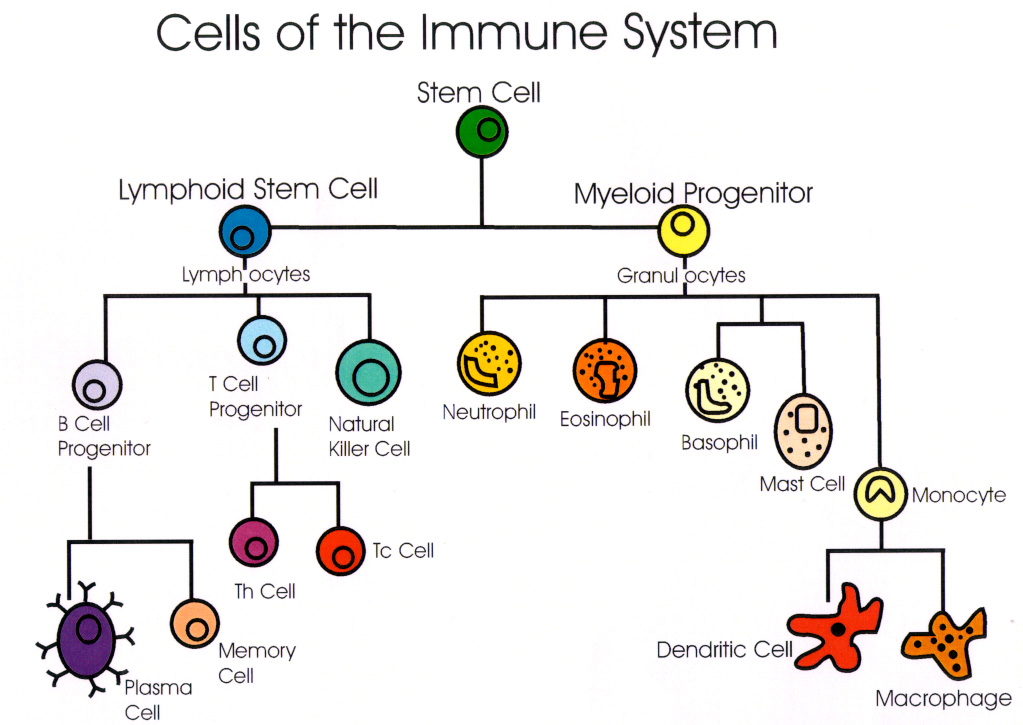
T-helper cells (Th) are a vital part of the immune system. They are a type of white blood cells that recognize and tag foreign pathogens. In response to this recognition, they produce cytokines (hormonal messenger proteins).
Th1 cells are involved in “cell-mediated” immunity, which deals with infections by viruses and bacteria that can get inside our cells (intracellular). As a result, they tend to be pro-inflammatory and are involved in the development of organ-specific autoimmune disease.
Th2 cells are involved in “humoral-mediated” immunity. This system deals with bacteria, toxins, and allergens. They stimulate production of antibodies in response to extracellular pathogens (found in blood or other body fluids). Typically, they are involved in systemic autoimmunity and other chronic conditions.
In a well-functioning immune system, both types of T helper cells work together to keep the system balanced. As a result, one side might become more active temporarily to eradicate a threat, then settle back to a balanced level.
Generally speaking, certain autoimmune conditions present as either Th1 or Th2 dominant. However, there can often be exceptions. Autoimmune conditions are not cookie-cutter! Luckily, there is a Th1/Th2 cytokine blood panel that your doctor can order to find out if your immune system is imbalanced.
| Th1 Dominant Conditions: | Th2 Dominant Conditions: |
| Type I diabetes | Lupus |
| Multiple sclerosis | Allergic dermatitis |
| Hashimoto’s thyroiditis | Scleroderma |
| Grave’s disease | Atopic eczema |
| Chronic viral conditions | Sinusitis |
| Rheumatoid arthritis | Inflammatory bowel disease |
| Lichen planus | Asthma |
| Crohn’s disease | Cancer |
| Sjogren’s Syndrome | Ulcerative colitis |
| Psoriasis | Allergies |
| Celiac disease | Multiple chemical sensitivity |
Antinuclear Antibody (ANA) Blood Test
There is a simple and inexpensive blood test you can do to see if autoimmunity might be underlying your symptoms. ANA is a general test; it does not reveal a diagnosis. However, if ANA is positive, you may like to do a comprehensive antibody screen to gain further insight. The ANA Profile 12 panel is available to answer more questions concerning the target tissue and a particular diagnosis.
Some of the diagnoses that might be revealed include…
- Systemic lupus erythematosus (SLE): SLE (lupus) is an inflammatory disease. It causes joint pain, fever, weakness, fatigue, skin rashes and organ damage.
- Scleroderma: Scleroderma is a rare disease that causes abnormal thickening and hardening of your skin and tissues. It can also affect your gastrointestinal tract, lungs, kidneys, heart, blood vessels, muscles and joints.
- Polymyositis: Polymyositis is a disease of the muscles that causes inflammation and weakness. It usually affects the muscles closest to your trunk.
- Dermatomyositis: Dermatomyositis occurs when people have disease features of polymyositis and also skin involvement such as a scaly rash, swelling and purple spots.
- Mixed connective tissue disease (MCTD): MCTD shares features with SLE, scleroderma and polymyositis. Usually, the symptoms of these diseases don’t occur at the same time. Rather, they occur one after the other over a long period of time.
- Juvenile onset idiopathic arthritis (JIA): JIA is a type of arthritis that may affect the joints in a variety of ways in your child’s body. Their hands, wrists, knees and other joints may be affected. It may also affect other parts of your child’s body, including their skin, eyes, lungs, heart and blood.
- Sjögren’s syndrome: Sjögren’s syndrome is a condition that reduces the amount of moisture produced by the glands in the eyes and mouth. The immune system damages the tear system in the eyes and the salivary glands in the mouth.
Keep in mind that regardless of the type of autoimmunity, there are certain anti-inflammatory strategies that are always recommended.
Favorite Supplements for Non-Organ-Specific Autoimmunity

Echinacea Premium – is recommended for most but not all people. It’s ok for those who already have a balanced Th1/Th2 system, or when Th1 is low/Th2 is high. Because Echinacea works slowly over time, it is best to take just a little bit, consistently. In other words, it’s not the best herb to take at a high dose for an acute infection.
Spleen PMG – this is a specialized bovine spleen extract. It provides the basic building blocks for spleen growth and repair. In addition, it is considered the “master PMG”, as the spleen houses the memory center for the immune system.
Thymus PMG – provides a blend of minerals, nucleotides, and peptides. These nutrients support proper functioning of the thymus gland. As the thymus reduces in function naturally as we age, this product can help strengthen or normalize the control center of the immune system.
Other Nutrients and Supplements for Autoimmunity and Lupus
| Th1 Stimulating Compounds: | Th2 Stimulating Compounds: |
| Astragalus | Caffeine |
| Echinacea | Green tea extract |
| Medicinal Mushrooms (Maitake & Beta-glucan) | Pine bark extract |
| Glycyrrhiza (from Licorice) | White Willow bark |
| Melissa Officinalis (Lemon balm) | Lycopene (tomatoes) |
| Panax Ginseng | Resveratrol (grape skin, sprouted peanuts, cocoa) |
| Chlorella | Pycnogenol (French maritime pine bark, apples) |
| Grape seed extract | Curcumin (turmeric) |
| Genistein (in soybeans) | |
| Quercetin (onions, berries, and kale) |
Final Thoughts on Autoimmunity and Lupus
Lupus presents a mix of symptoms that could seem vague and unrelated. However, it’s important to fully understand your symptoms. There could be a connection to autoimmunity. Understanding your unique set of symptoms and doing the right testing can lead to a proper diagnosis and effective nutritional support. As a result, you can feel better and improve your quality of life for many years to come! Above all, find out more information if you have been struggling.
Let us know how we can help!