By Claire Bacon, ACN, CNC
All too often, when a couple has difficulty conceiving, we immediately look to the woman’s health. What is up with her hormones? Is she too stressed out, working out too much, or not eating enough? So much attention gets placed on the woman. Meanwhile, what’s happening with the man out of the spotlight? What’s up with his health? Maybe we should change the narrative, and pay closer attention to the other 50% of the DNA required for conception. Let’s explore all the things we can do naturally to support male fertility.
Some Disturbing Statistics
First, let’s consider the situation from a bird’s eye view. In the United States, our fertility rate is below replacement level (about 1.6 children per woman in 2024, vs. the replacement level of 2.1). And globally, fertility is declining nearly everywhere, though at different speeds and from different starting points.
Part of this is because people – both men and women alike – are waiting longer to have children due to careers, education, access to contraception, etc. and of course we know advanced age is a huge factor. But what’s really disturbing is that some studies show declining sperm counts in Western men over the last 40 years (over 50% drop in some meta-analyses).
- Reasons for worldwide decline in male fertility
- Temporal trends in sperm count
- Are sperm counts really declining?
- Sperm counts and fertility in men: a rocky road ahead
And it’s not just a lower sperm count—there is also much worse motility and morphology, especially in Western countries.
Fertility Rates and Trends
Let’s take a look at the Total Fertility Rates (TFR) in the United States by decade, from the 1950s through the 2000s. These rates represent the average number of children born per woman over her lifetime.
| Decade | Total Fertility Rate (TFR) | Notes |
| 1950s | ~3.5 (peak ~3.7 in 1957) | This was the Baby Boom era, with high post-WWII birthrates. |
| 1960s | ~3.0 to 2.5 | A slight decline began in the mid-sixties; following the birth control pill being introduced in 1960. |
| 1970s | ~2.5 to 1.8 | Birth rates continued to drop; in 1972 the U.S. fell below replacement level, possibly a result of extended tensions concerning the Vietnam War and Cold War. |
| 1980s | ~1.8 to 2.0 | Stabilized birthrates, slight rebound from 1970s low, possibly a reflection of a more hopeful and positive political and cultural climate. |
| 1990s | ~2.0 to 2.1 | Hovered around replacement level (2.1); with slightly lower birthrates coming from White Americans, higher birthrates coming from higher immigration rates. |
| 2000s | ~2.1 to 2.0 | Rates hovered near replacement level through most of the decade; with a slight decline after 2007. |
| 2010s | ~1.84 → 1.69 | A continued steady decline: ~1.93 in 2010, ~1.86 mid‑decade, ~1.69 by 2019 |
| 2020s | ~1.64 → 1.62 | Dropped to ~1.64 in 2020, slight rise to ~1.66 in 2021; historic low ~1.62 in 2023, possibly reflecting a lasting health consequence of Covid. |
Fertility Rates Lead to Questions
These relatively low birth rates are not particularly new, as birth rates have been low approximately 20 years. But it is very concerning that the lowest rate measured occurred as recently as 2023. Could this point to the Covid pandemic as having an impact to our collective sperm and egg health?
On top of these low rates, couples seeking fertility assistance from Reproductive Endocrinologists has gone up. In 2006, approximately 140,000 assisted reproductive technology (ART) procedures were performed; producing 55,000 babies. Compare that to 2023, with almost 400,000 IVF procedures and 95,000 babies born from ART. IVF and other types of ART now represent about 1.5–2% of all U.S. births.

What Determines Male Fertility? A little anatomy…
There are two main factors that determine a man’s sperm count. These are the number of Sertoli cells in his testes and the number of days since his last ejaculation. Note that abstinence is variable and within a man’s control, whereas the Sertoli cell number is fixed, and is determined as a man develops through puberty.
Sertoli cells are the supporting cells of the seminiferous tubules – the coiled structures where sperm are produced within the testes. The tubules contain Sertoli cells, spermatogenic cells, and Myoid cells (to help sperm move through the tubules.
The Sertoli cells provide nutrients, support phagocytosis, and maintain the blood-testes barrier for the developing sperm. Testosterone is a major driver of the Sertoli cell functions.
Men also have Leydig cells in the testes, which are not located inside the seminiferous tubules. They are found in the spaces between the tubules, called the interstitial tissue of the testes. Leydig cells are the primary producers of testosterone in men.
How Does It All Work?
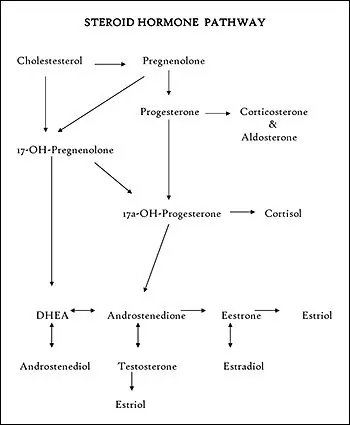
- The hypothalamus gland (perception center, sensitive to stress) releases Gonadotrophic Releasing Hormone (GnRH) to stimulate the pituitary gland.
- The pituitary gland produces Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH), which stimulates the Leydig cells to produce testosterone.
- The resulting testosterone stimulates the Sertoli cells to support sperm production.
- The actions of testosterone and Leydig cells also develop the secondary sex characteristics, such as a lower voice, muscle building, and heightened libido.
- Testosterone and the Leydig cells help to maintain bone density, energy, and red blood cell production.
- When testosterone is plenty high, the hypothalamus down-regulates its GnRH to slow down this cycle of production.
Areas of Vulnerability
Now that we understand the physical process of generating sperm, we can see several key points that might disrupt the system and impact fertility:
1. Endocrine disrupting chemicals (EDCs) present during puberty.
This is the time when the Sertoli cells and the blood-testes barrier are forming. So, any chronic toxicity during this time potentially has a profound effect on future fertility capacity. Examples include:
- BPA (plastics),
- Phthalates (personal care products like deodorants, cologne, and body sprays),
- Pesticides (DDT, atrazine),
- PFAS (non-stick cooking pans and waterproof materials)
- Heavy metals (lead, cadmium, mercury, etc.)
2. EDCs can impact a man’s hormonal receptors at any time during his life.
These chemicals mimic or block hormones like testosterone, FSH, and LH. They confuse the endocrine system and prevent normal physiology from working.

3. Stress and poor sleep influencing the performance of the hypothalamus gland.
The hypothalamus is always picking up cues from our internal and external environments. It is easily downregulated by intense or chronic fear and stressful situations. Even a chronic lack of sleep is a major stressor on the hypothalamus. It’s the only time we’re truly in growth and repair!
4. Nutritional deficiencies affecting the actions of the hypothalamus, pituitary, and testes.
The most important nutrients for male hormonal functions are: zinc, selenium, vitamin D, iodine, omega-3s, all the B vitamins, and vitamin A. When these nutrients are low, a man can have inadequate hormone synthesis, impaired testicular growth and sub-par sperm production.

A few more common factors…
In addition, we also know a few more common factors that can play into male fertility:
- Physical injury to the testes, such as from a kick, bicycle accident, or sports trauma, can temporarily affect fertility, but permanent infertility is relatively rare. Even with a severe injury, one healthy testis is usually enough for normal fertility and hormone levels.
- Metabolic issues like obesity and insulin resistance can spur the aromatase enzyme to convert testosterone into estrogen.
- Heat exposure from saunas and hot tubs can quickly kill the “ready and waiting” sperm.
- Recreational drug use. Alcohol is bad, but marijuana is even worse. (Can you imagine your sperm “vegged out” on the couch?)
- Anabolic steroids used with muscle building turn on the “negative feedback loop” mentioned above. With excess testosterone in the system, there is no need for the testes to be active, and so they shrink and atrophy.
- Infections and inflammation. Childhood mumps are well-known to impact the health of the testes. Later in life, getting a STD like chlamydia or gonorrhea could do the same. We are starting to understand the recent impacts of Covid infection on the testes; hopefully the coming years will reveal effective strategies to deal with lingering inflammation from Covid, as well as the shots.
- Oxidative stress impacting the mitochondrial functions of the sperm, testes, and body as a whole.
Top 10 Solutions to Male Fertility
So, now that we have our eye on the problem, what can we do about it?
#1. Don’t delay because of your ego.
You are not a failure, and no one is judging you. We just want you to get checked out! We know men don’t like going to the doctor. You’d much prefer to just stick your head in the sand and pretend everything’s fine. Well, now you’re doing yourself a disservice, and you’re wasting your wife’s precious time. This process of checking out your fertility is not a threat to your masculinity. It is an acknowledgement that you’re in it for the long haul, matching her commitment 100 percent. Let’s do this!
#2. Check out your inflammatory factors and all the basic bloodwork markers.
You need to know if you’re part of the 88 percent of Americans who aren’t metabolically healthy. Chat with Dr. Bacon if you need help getting your blood tests run.
#3. Get a semen analysis and a physical exam of your testicles.
You need to know if you have varicoceles, sooner rather than later, because these might need surgery. Don’t be afraid to get examined. Women have been subjecting themselves to “inspections” ever since puberty!
#4. Eat a nutritious, organic diet.
You’ll want loads of brightly colored, fresh fruits and vegetables with high antioxidant content. (More about this below).

#5. Add supplements according to your unique needs.
You don’t know what you need if you don’t test! We have lots of ways to figure out what your body is lacking, and how you can start feeling better right away. Come see Dr. Bacon and Claire for more guidance.
#6. Clean out your personal care products.
Clean out your medicine cabinet and eliminate unnecessary meds, too. You don’t need all the OTC drugs. It’s time to get healthy – naturally!

#7. Stop using exogenous testosterone.
It suppresses your natural sperm production. Note that you may need to add HCG or Clomid to wake up sleeping testes.
#8. Get daily movement.
Especially resistance exercise is so beneficial for boosting your testosterone. Work hard, and you’ll get an even better night’s sleep. It’s the only time you’re truly in a growth and repair process!

#9. Grow up and stop partying so much.
Alcohol and marijuana (and probably vaping, too) are much more harmful than you think! Not only do they cause inflammation and liver toxicity, but they dampen mitochondrial processes and cut down on your gut microbiome, as well.
#10. Time your intercourse properly.
Best chance of conception occurs with having sex every 1–2 days the week of her fertile window.

Best Nutrition for Male Fertility
The most helpful nutrients for male fertility include zinc, selenium, vitamin D, vitamin B12, folate (B9), CoQ10, L-carnitine, vitamin E, vitamin C, omega-3 fatty acids, magnesium, arginine, glutathione, and iodine. These nutrients support healthy testosterone levels, sperm production, motility, DNA integrity, and protect sperm from oxidative stress.
Now let’s get these nutrients from our food…
- We want to include: oysters, beef, and pumpkin seeds for zinc;
- Brazil nuts, eggs, tuna, and sunflower seeds for selenium;
- cod liver oil, salmon, and fortified milk for vitamin D.
- Clams, eggs, dairy, and meat provide vitamin B12,
- leafy greens, legumes, and liver are rich in folate.
- For antioxidants like CoQ10 and glutathione, focus on sardines, organ meats, asparagus, avocado, and cruciferous vegetables.
- Red meat, dairy, and avocado supply L-carnitine,
- almonds, sunflower seeds, spinach, citrus fruits, strawberries, and bell peppers offer vitamin E and C.
- for hormone balance and sperm membrane health, eat fatty fish like salmon and mackerel, walnuts, flaxseed, and dark chocolate.
- Finally, include chickpeas, turkey, lentils, eggs, dairy, and seaweed for magnesium, arginine, and iodine.
Yes, we do have a recipe packet that includes many of these foods for male hormonal balance! Click this link to download!

And of course, a few essential supplements…
- Ashwagandha Complex has a unique blend of herbs to give you the “strength of a stallion”. Contains Ashwagandha, Licorice, Skullcap, and Korean Ginseng.
- Orchic PMG is a specialized extract used to promote normal growth and repair of the orchic glands (the testes).
- Tongkat Ali is a very helpful herb when we know that SHBG is high, and free testosterone is low. Tongkat Ali helps to correct this imbalance so you can feel more vigor and vitality.
- B-Vital is a male enhancement blend of Peruvian Maca and Velvet Deer Antler. These herbs are used to restore balance and increase energy and stamina.
Final Thoughts
Male fertility can be influenced by many factors—some beyond your control, but many well within your reach. From hormone imbalances and environmental exposures to nutritional deficiencies and lifestyle habits, there are numerous potential obstacles to optimal reproductive health. The key is to get tested and identify which areas need the most support. Armed with that knowledge, you can take clear, targeted steps to improve your fertility, boost hormone health, and protect long-term vitality.
Fertility isn’t just about starting a family—it’s a reflection of your overall health. The next step is to take action.


