By Claire Bacon, ACN, CNC
Diabetes is one of the largest health threats in our society today. Diabetes is a chronic disease involving high glucose in the blood. It can be caused by inadequate production or utilization of insulin. This can occur because of different triggers, resulting in various protein and lipid metabolic disorders. Sometimes there is an autoimmune aspect to the disease, where the immune system attacks pancreatic cells and results in Type 1 Diabetes (T1D). This requires an additional level of support, to modulate the immune activity and keep inflammation low.
In the United States, the statistical occurrence of T1D is 20 per 100,000 people. Across the world, it is estimated to be 15 per 100,000 people. But we are a wealthy country. Why is our health not better? Why is the incidence of T1D worse in the United States? Maybe it has something to do with our diet? Or could it be something more?
The SAD Standard American Diet and T1 Diabetes
In our Standard American Diet (SAD), processed foods and grains dominate the grocery store landscape. These foods have been promoted by government regulations and food manufacturers ever since the development of the Food Pyramid in 1992. The food pyramid placed major emphasis on consuming grains and carbohydrates, which create a high insulin response. At the same time, the food pyramid recommended limiting fats (even healthy fats), which don’t provoke a change in insulin. Most of you probably remember the influx of low-fat and fat-free packaged items that flooded store shelves in the early 90’s.
The Standard American Diet includes a lot of added sugars, fructose, and specifically, high fructose corn syrup (HFCS). Added sugars provide flavor for foods that don’t have the healthy fats and minerals we would get from natural foods. As a comparison, across the world high fructose corn syrup occurs in about 8 percent of added sugars; whereas in the US it is in 42 percent of our processed foods. What a difference!
Food manufacturers utilize HFCS to sweeten foods because it is cheaper than real sugar. Other names you may see on the label include: corn syrup, corn syrup solids, dextrose, glucose, or sucrose. All of these are bad for you. Why? Because they all induce a high glycemic response, which requires insulin from the pancreas to bring it back down. Over time, frequent glucose and insulin spikes can fatigue the pancreas and the rest of your hormonal system.
A Healthier Diet for T1 Diabetics
At some point, everyone needs to come to a realization that we can either follow the government guidelines for a grain- and starch-heavy diet, or we can go back to what our ancestors did back in the day when almost everyone was healthy. Which will it be for you? To eat more grains and sugar, or eat more meat and fat? You can probably guess where we’re going with this one. 🙂
With diabetes, the key to a healthy diet is to lower inflammation. Diabetics’ bodies are ON FIRE with inflammation. We know that part of this fire is because of sugar and things that metabolize like sugar, like wheat, other grains and starchy carbohydrates, and alcohol. Of course we also know that stress and high Cortisol play a part. And in the next section we’ll discuss chemical exposures that disrupt our metabolism. Long story short, diabetics need special dietary considerations. Here’s a short summary…
- Ketogenic diet
- Timing of Meals
- Choose foods the way Nature made them
- Go walking after a meal
- Avoid potential sensitivities
- Supplement thoughtfully.
Ketogenic Diet
The key thing to understand with diabetes is the body can’t handle carbohydrates properly. Type 1 diabetics are not producing enough insulin from the pancreas, so every meal makes glucose go high, and nothing can bring it down until you add exogenous insulin. The period of time when glucose is high is very destructive. Small capillaries (especially in the eyes and kidneys) get inflamed and less functional with the continued onslaught of high glucose. That’s why a Ketogenic diet is so helpful. We recommend a dairy-free Ketogenic diet, because milk protein can be harmful to the pancreas. Eating meat, eggs, lettuce, non-starchy veggies, and healthy fat is filling, nutritious, and doesn’t cause a glucose spike.
Timing of Meals
In addition to WHAT you eat, the question of WHEN you eat becomes very important. Diabetics need to monitor their glucose closely. If they are insulin-sensitive and just not producing enough, they need to stay on top of the hourly fluctuations and not let glucose get too high or too low. Timing of meals becomes very important if you’re having trouble keeping glucose stable or getting a good night’s sleep. For those people who might be insulin resistant, blood sugar might be staying too high for too long. This can happen even with proper use of insulin, and some other medications might be necessary to help. In this case, intermittent fasting and going long periods of time without eating could be very helpful to reduce inflammation.

Choose Foods the Way Nature Made Them
Yes – the way Nature made them! As in real food – not processed in a factory! We all need to return to this concept of eating how our ancestors did. For diabetics, it may be even more important, because modern chemical additives like dyes, sweeteners, and preservatives may have detrimental effects on our metabolism. That’s right, even Nutrasweet and Sucralose that are marketed towards diabetics may still be bad for you. It’s not the calories, it’s the chemicals!
Go Walking After a Meal
Maybe you’ve heard that going for a walk after dinner is good for your digestion. Quite possibly, you’ve heard that it helps to reduce a glucose spike. And this even holds true for diabetics! Doing light activity will have a beneficial effect in lowering your post-prandial blood sugar. This is even more evident with higher intensity or a longer duration effort. Diabetics need to pay close attention to make sure their blood sugar doesn’t go too low.

Avoid Potential Food Sensitivities
Many people dealing with diabetes are also dealing with a leaky gut. As such, they may have multiple triggers for inflammation and maybe even some troubling gut issues. Anytime we find someone with autoimmunity, we recommend the Autoimmune Protocol Diet. It’s the best plan when you need to lower your gut inflammation, but still want a decent list of foods you can have. On the avoid list: gluten, dairy, corn, and soy; nightshades like peppers, tomatoes, white potatoes, and eggplant; eggs, nuts and seeds; and beans and legumes. What’s left? Meat, lettuce, some vegetables, and fruit.
Supplement Thoughtfully
By this time, you’ve probably figured out that we can’t get all the nutrients we need from our food. That’s when we need to supplement! Choosing high quality, therapeutic vitamins can make a huge difference in how you feel. Get the advice you need – give us a call!
- B Vitamins like Thiamine are often lacking with diabetes. Our first choice for a good supplement would be Cataplex B, because it has thiamin along with choline and inositol.
- Magnesium deficiency can increase the risk for cardiovascular issues concurrent with diabetes. We suggest EZ-Mg because it’s sourced from kale, Swiss chard, and beet leaf greens, and is also a good source of Potassium for the adrenals.
- Gymnema has been the subject of many studies, exploring its potential benefits for rejuvenating the Beta cells in the pancreas with long-term use.
- Lipoic Acid Plus has a variety of metabolic benefits, including better liver function and a glucose-lowering effect.
- Berberine Active not only has benefits for blood sugar control, but also can be good for gut dysbiosis and clearing out unwanted bacteria.
- Olprima EPA/DHA provides the key anti-inflammatory essential fatty acids, EPA and DHA, in a concentrated dose.
Environmental Factors Increase Risk
Research studies suggest that a number of factors could play a role in T1D besides diet, including: vitamin D status, environmental chemicals, early childhood infections, and the gut microbiome. Certainly these things need our attention and can be within our control to make improvements.
One of the worst chemicals that we’re constantly exposed to is Glyphosate. It’s the active ingredient in Roundup, which is an ubiquitous pesticide used widely across our farmland. Take a look at the increase in Roundup usage ever since 1996 when GMO-ready crops were introduced…
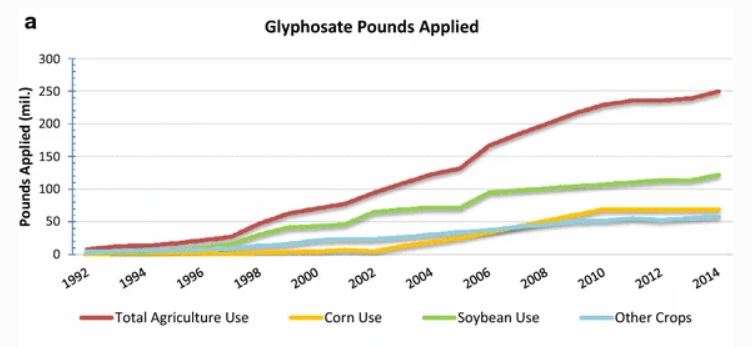
Sadly, this increase in pesticide usage is unavoidable. Even if you’re choosing organic foods every time you shop, restaurants are using conventional, pesticide-sprayed foods. So we’re all being exposed to glyphosate and other pesticide chemicals on a regular basis. And studies show that increased organochlorine pesticides can damage our gut microbiome and lead to chronic disease, including T1D.
Where else do we encounter environmental chemicals? Consider these common exposures:
- Childhood vaccines & yearly flu shots
- Lawn treatments
- Contaminants in tap water
- PCB pollutants
- Polycyclic Aromatic Hydrocarbons (PAHs)
- Bisphenol A and Bisphenol S
- Phthalates
- Flame retardants
- Dioxin contamination
- Perfluorinated alkyl substances (PFAS)
It’s hard to know what chemical exposures may have been in our past, but we do have testing to look at what chemicals may still be present in the system. We recommend the Toxic Metals and Elements (TME) saliva and urine test from Diagnostechs. And as an alternative, we have the MOE-TOX test available from US Biotek. Toxic exposures may require some specific measures for removal and detoxification.
The Autoimmune Aspect of T1 Diabetes
Type 1 diabetes (T1D) is caused by an autoimmune-induced inflammatory destruction of the pancreatic tissue. Specifically, it’s the Beta cells in the pancreas that are affected by the autoimmune activity.
There are some specific screening biomarkers you can look for in the blood. Biomarkers of beta cell autoimmunity in T1D are:
- islet cell autoantibody (ICA)
- glutamic acid decarboxylase (GAD)
- insulin autoantibodies (IAA)
- protein tyrosine phosphatase (IA-2A).
In addition, we know that diabetics commonly are low in certain nutrients. That’s why we also recommend checking for: B vitamins, magnesium in the RBC, potassium, vitamin D, and Omega 3:6 fatty acids.
The early occurrence of autoantibodies is associated with a greater risk for T1D. Antibodies may appear months or even years prior to symptoms. In young children, the first one to appear is insulin autoantibody (IAA). IAA is present in approximately 70% of diabetic children at time of diagnosis.
Like all autoimmune conditions, T1D originates with dysfunction within the gut lining. And as such, it is very common for one autoimmune condition to lead to more. If you’ve been diagnosed with T1D, you should consider whether any other autoimmune conditions may be contributing to your symptoms. Maybe not everything you’re feeling may be related to insulin and sugar?

Other Autoimmune Markers
LabCorp provides a wide variety of antibodies available to order. Note that sometimes one antibody marker may be present for a condition, but another related antibody may not. Remember, if you have lots of autoimmunity showing up, that relates to how “leaky” or permeable your gut lining is.
It’s not common to check these antibodies, but they are available and may be worth exploring, depending on the symptoms you’re feeling:
Thyroglobulin & Thyroperoxidase for Graves’ & Hashimoto’s thyroiditis
Zinc Transporter 8 (ZnT8) antibodies
TSH Receptor (TRAb or TSHR-Ab) can either stimulate or inhibit thyroid hormone production
Anti-Transglutaminase IgA (tTG2) for Celiac
Intrinsic Factor blocking antibodies for pernicious anemia, autoimmune gastritis
Deamidated gliadin peptide antibodies (anti-DGP) for Celiac
Anti-endomysial antibodies (anti-EMA) for Celiac and dermatitis herpetiformis
Antinuclear Antibodies (ANA) for Sjogren’s, Lupus, and other autoimmunity
Double-stranded DNA (anti-dsDNA) for Lupus & connective tissue diseases
Glutamic acid decarboxylase (GAD) enzyme produced in pancreas, creates GABA
Antipancreatic Islet cell antibodies
Adrenal Cortex antibodies for Addison’s disease
IgA and IgG Anti-Gliadin antibodies (AGA) for gluten sensitivity
Parietal Cell antibodies against the stomach cells (APCA)
Cyclic citrullinated peptide (CCP) for RA
Anti-Ro/SSB, Anti-La/SSB (ribonucleoproteins) for Sjogren’s, Lupus, and other autoimmunity
Smooth muscle (ASMA) against the liver
In addition, or either/or, you may like to run a comprehensive food sensitivity test. The best ones (ELISA tests) use a combination of IgE and IgG markers, or may differentiate between cooked and raw foods. Surprisingly, this can make a difference to how your gut handles the food!

Our Holistic Strategy for T1 Diabetes
If you have autoantibodies, then we know there is some level of immune dysregulation in the gut. In the holistic world, our guiding principle is that “all autoimmune disease begins in the gut.” Therefore, our autoimmune strategy will always involve:
- avoidance of inflammatory foods that irritate the gut, such as refined carbs with chemical preservatives, or even nightshade vegetables.
- specifically for diabetes, avoidance of gluten, dairy, and sugar are paramount
- elimination of pathogenic yeast, bacteria, mold, and parasites in the gut
- healing of the leaky gut lining with nourishing food, supplements, and probiotics
- use of anti-inflammatory herbs and nutrients, such as Turmeric and Fish Oil
- use of pancreas-restoring enzymes and herbs, most notably Gymnema
- use of immune system decoys (protomorphogens like Pancreatrophin PMG) and immunoglobulins (like Immuno-gG-SBI).
We have written extensively about each of the above items. Click the embedded links so you can learn more about these topics! These concepts are not necessarily only for diabetics, and are not only for autoimmune conditions, either. We are explaining our holistic philosophy of whole-body nutrition, which leads to whole-body health!
Clearly, there are many things you can do to reduce your risk and increase your function. We know that this can seem daunting. That’s why we always recommend working with a professional team of a Nutritionist with your Chiropractor and other holistic practitioners to keep an eye on the big picture of your health.


